Sept. 5, 2023 – You may have heard of the three most common forms of skin cancer — basal cell carcinoma, squamous cell carcinoma and melanoma — but there is a rarer and deadlier form known as Merkel cell carcinoma.
The passing of popular singer and songwriter Jimmy Buffett, who died Friday at age 76 from Merkel cell carcinoma, has thrust this form of skin cancer into the spotlight. But what exactly is it? What are the warning signs, how different is it from other skin cancers, and how does it cause death?
WebMD reached out to one of the preeminent experts on Merkel cell carcinoma for answers: Paul Nghiem, MD, PhD, chair of dermatology at the University of Washington School of Medicine and director of the Skin Oncology Clinical Program at Fred Hutchinson Cancer Center, both in Seattle. We also sought the expertise of Travis Blalock, MD, director of dermatologic surgery, Mohs micrographic surgery and cutaneous oncology at the Emory University School of Medicine in Atlanta.
Greater awareness about this type of skin cancer is important, Nghiem said.
“There is another skin cancer besides melanoma, squamous cell carcinoma, basically the more common ones that one hears a lot about. This cancer is more than four times more likely to kill somebody than a melanoma.”
Blalock agreed: “Merkel cell carcinoma is an uncommon yet sometimes highly aggressive form of skin cancer.” About 2,500 cases are reported each year in the United States. The lesions typically appear on the head, neck, arms and legs, the parts of the body that get more sun exposure.
Not an Obvious Cancer
When asked how easy or difficult it is to diagnose Merkel cell, Nghiem replied, “I would say for the average person, impossible. For an excellent dermatologist, very difficult. But a good doctor will know something unusual is going on and order a biopsy.”
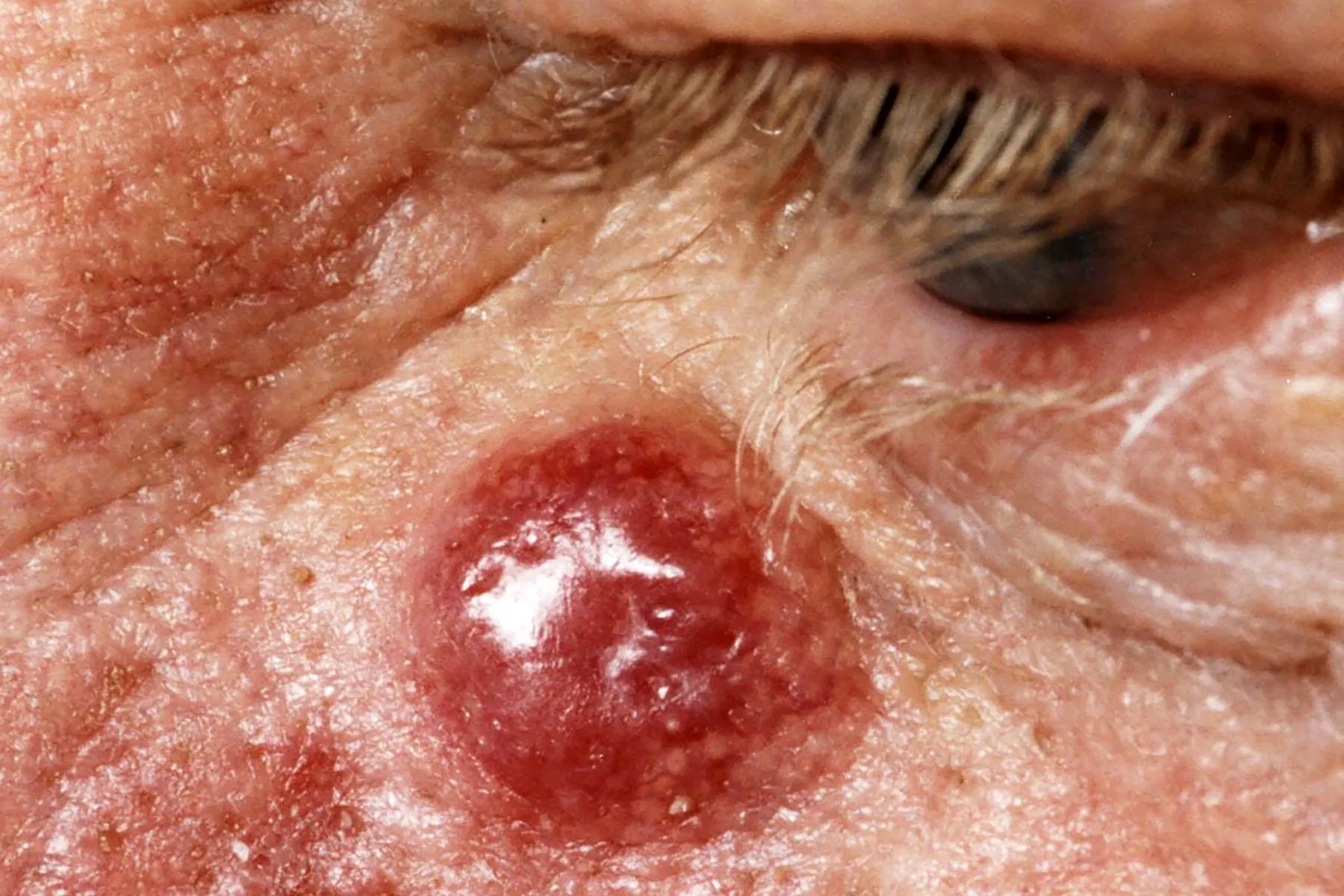
While many people know a dark-colored lesion can mean melanoma, spotting MCC can be more challenging. “Merkel cell carcinoma can sometimes present as a nondescript, rapidly growing tumor with a red or pink appearance,” Blalock said. “Unlike melanoma, it lacks a well-known characteristic color.”
A Merkel lesion on the skin can be easily mistaken for a bug bite, a sore, a cyst, or a pimple. However, Merkel cell carcinoma usually grows quickly and is not tender to the touch.
Consider the A-E-I-O-U mnemonic:
- A is for Asymptomatic (does not hurt)
- E is for Expanding (rapidly growing)
- I is for Immunity (impaired immunity can mean higher risk)
- O is for over 50 years old
- U is for UV exposed skin
About 90% of Merkel cell patients have three or more of these factors.
A Viral Cause
The reason people with compromised immunity can be at greater risk is that Merkel cell carcinoma is, in about 80% cases, caused by a virus. That’s another way it differs from other skin cancers. The remaining 20% of cases are associated with sun exposure. In many cases, it’s the combination of these two factors that somehow lead to Merkel cell.
“The virus is crazy because it’s on most of our normal skin most of the time. So it’s a very, very common virus and a very rare cancer,” Nghiem said. “That’s an unusual combination.”
How sun exposure and the virus work together to cause this cancer is not fully understood. But people with darker skin tend to have lower risk, and “that’s clearly telling us there’s an interaction between the sun and this virus,” he added.
The goal is to catch Merkel cell carcinoma and other forms of skin cancer earlier, before they have the chance to spread to other parts of the body. More than 50% of Merkel cell patients experience lymph node metastasis and about 30% see the cancer spread to other organs.
It’s Complicated
Researchers do know a complicated series of steps has to take place for Merkel cell carcinoma to develop.
“There are genetic mutations that need to happen, and we now understand those quite well. The DNA of the virus needs to get into the cancer cell and get chopped up in a certain highly specific way, and then that leads to the cancer,” Nghiem said.
That could be a silver lining. “If it weren’t that complicated, this would be enormously more common because basically everyone gets some sun and everybody has exposure to this virus,” he added.
The Skin Cancer Foundation estimates than 1 in 130,000 Americans will be diagnosed with Merkel cell carcinoma. In addition to the immunocompromised, people most at risk include those with a history of sun exposure, those with fair skin, and those who are older than 50.
Although relatively rare, the number of Americans diagnosed with Merkel cell carcinoma is growing “much faster than other types of cancer, and melanoma in particular,” Nghiem said. The aging of the American population, including many who seldom used sun protection, could be behind the increase in cases, the American Academy of Dermatology says on their website.
Merkel cell carcinoma often spreads to other parts of the body if not caught early enough. If it appears on the head or neck, for example, it tends to go to the liver. Merkel cell lesions on the legs and other parts of the body typically spread to the lymph nodes around the gut.
If a biopsy comes back indicating this rare cancer, seek care at one of about a dozen specialty centers around the country if you can, Nghiem suggested.
“There’s clear evidence that survival outcomes are better if you go to a center that’s familiar with how to manage it.” The site Merkelcell.org offers a nationwide list of specialists.
Although the cancer is relatively rare, ”if you’ve had other skin cancers and you’re immune-suppressed following an organ transplant, for example, it’s really important to get watched carefully,” Nghiem said. “Not just for this alone, but for all skin cancers.” For people on lifelong immune suppression, the risk for Merkel cell carcinoma jumps by 30 times, he added.
Newer Therapy Offers Hope
If caught early enough, before it spreads to other parts of the body, Merkel cell carcinoma can be treated successfully in many cases.
Another tip is to ensure your health care provider suggests radiation treatment. Unlike many cancers than “grow into a ball” that can be removed with surgery, Merkel cell carcinoma jumps locally and distantly around the body, known as “microscopic spread.” So radiation is a preferred treatment in many cases because it can treat a larger region than surgery. Radiation also kills the tumor cells in Merkel cell carcinoma more effectively than it does in some other types of cancer.
A newer treatment strategy, immunotherapy, is a more targeted treatment based on a person’s unique genetic mutations. It can be more effective than traditional treatments like chemotherapy because chemotherapy tends to knock out the immune system, which again raises the risk for Merkel cell carcinoma.
“Immunotherapy is making a huge difference. The chance of surviving is now about 10 times better,” Nghiem said.
The multiyear survival has increased from about 5% to about 50% today, he said. The American Cancer Society offers estimates for 5-year survival, which vary depending on whether the cancer is local or has spread around the body.
The improved survival rates would be unlikely without the research support from the National Institutes of Health and the National Cancer Institute, Nghiem said. “That’s made a big difference, and it’s important for the public to know that.”
For rare conditions like this and many others, federal and national funding is particularly essential. Although one rare condition might affect relatively few Americans, together they add up to about 40% of diseases. He added, “When you look at the big picture, they’re a big deal.”
Blalock said he has witnessed significant advances in diagnosing and managing this “extremely dangerous cancer” during his dermatology career. “These developments have empowered us to intervene effectively and enhance the quality of life for patients who have historically faced a grave prognosis,” he said.